Cardiac MRI Study
The Cardiac MRI study has been ongoing since 2002. The goal is to understand brain development and risks of brain injury in babies with congenital heart disease. The results so far include:
 Figure: Normal Fetal Circulation and Changes with Congenital Heart Disease
Figure: Normal Fetal Circulation and Changes with Congenital Heart Disease
Course of blood flow in a late gestation fetus with normal heart anatomy (A), d-transposition of the great arteries (B) and hypoplastic left heart syndrome due to aortic atresia (C). Deoxygenated blood (blue-purple) flows to the placenta through the umbilical artery (UA) where gas exchange takes place. Blood with higher oxygen content (red) returns through the umbilical vein (UV) and ductus venosus (DV) to the inferior vena cava (IVC). The more highly saturated blood forms a stream in the IVC, which is preferentially directed across the foramen ovale into the left ventricle in the normal fetus and with d-TGA. Estimated hemoglobin oxygen saturation in percent is shown for each ventricle. Blood flow to the fetal lungs is limited by elevated pulmonary vascular resistance. In the fetus with d-TGA, the aorta arises from the right ventricle such that the brain receives less oxygenated blood, while the higher saturated blood is directed to the descending aorta through the ductus arteriosus. In HLHS, reduced or absent left ventricular ejection results in elevated left atrial pressure, limiting or reversing flow at the foramen and resulting in complete mixing of desaturated and well saturated blood in the right atrium and ventricle. Blood flow the head and neck may occur in a retrograde fashion from the ductus arteriosus across the aortic isthmus.
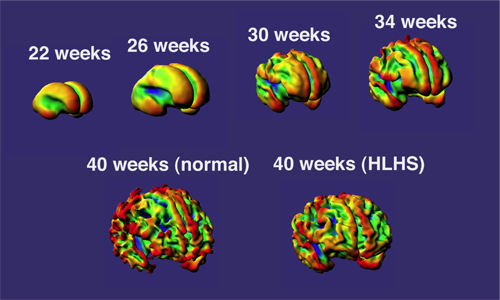
Currently we hypothesize that delayed brain development may put newborns with CHD at risk of white matter injury around the time of surgery. ‘White matter’ includes the connection between brain cells (neurons or ‘grey matter’) and the cells that produce ‘myelin’ to support and insulate the neurons. We are focused on identifying interventions or medications to prevent any brain injury around surgery. Selecting these interventions would not be possible without the information we have gathered from our study babies to date.
We are finding that children with heart disease repaired during infancy, share many aspects of behavior and learning styles noted at school age in children born prematurely. Both groups score within the normal range on IQ testing, but are challenged by tasks that require attention, executive function and visual-motor integration.
Our present focus includes fetal MRI to understand how brain development is affected by congenital heart disease before birth. We are also following infants and children after surgery to watch how they develop into school age and beyond to understand and achieve optimal brain development, or if needed, repair and recovery following newborn heart surgery.
