Advancing Alzheimer's Research Through Neuroimaging
Leighton Hinkley, PhD, first author of "Distinct neurophysiology during nonword repetition in logopenic and non-fluent variants of primary progressive aphasia" in Human Brain Mapping uses advanced imaging techniques to better understand neurodegenerative diseases. The research focused on Primary Progressive Aphasia (PPA), a condition within the Alzheimer's disease spectrum. In a recent interview Hinkley, a neuroscientist at the University of California, San Francisco (UCSF), explains his team's neuroimaging research.
The Motivation Behind the Study
"The study is the first of its kind," shares Hinkley, noting that it was prompted by a collaboration with experts in the Department of Neurology at UCSF's Memory and Aging Center, who have long grappled with the challenge of diagnosing diseases like PPA based solely on behavioral observations. In PPA, different subtypes can be challenging to distinguish behaviorally despite having distinct brain origins and pathological mechanisms. This dilemma motivated the team to explore non-invasive advanced imaging techniques to identify underlying patterns of brain activity that could improve diagnostic accuracy. Hinkley observed, "One of the exciting things about this study is that it really highlights what we can do with the tools that we have available."
Key Findings
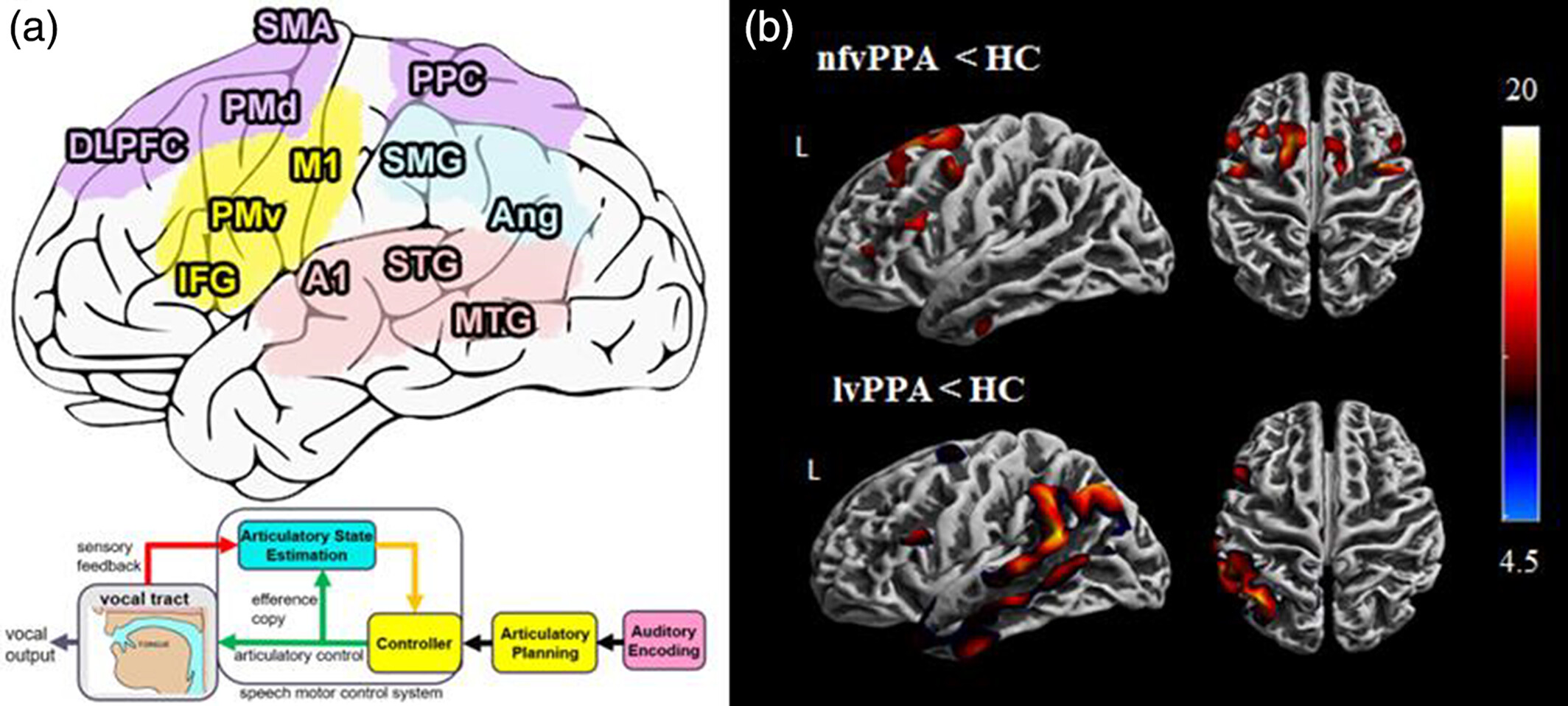
The study focused on two variants of PPA: the logopenic variant and the nonfluent variant. Hinkley's team found that each variant exhibited reductions in brain activity in specific regions that were not solely attributable to atrophy. This suggests that the PPA disease process involves structural changes and impairments in brain activity, and challenges the conventional understanding of neurodegenerative diseases.
To arrive at these findings, the team combined magnetoencephalography (MEG) with measurements of neurodegeneration obtained through MRI (magnetic resonance imaging). By merging MEG and MRI data, the team identified patterns of brain activity independent of brain atrophy. This is a crucial discovery as it implies that reductions in brain activity can occur before significant atrophy is detectable.
Hinkley emphasized that very few studies use MEG in Alzheimer's disease and related dementias: "A unique aspect of the study is this really cool high-tech machine – a MEG scanner – that we have at UCSF, which allows us to look at and localize frequency patterns of brain activity. We're able to identify a deficit of high-frequency activity in the non-fluent variants and a deficit of low-frequency activity in the logopenic variants." These findings, made possible by MEG, provide insights into PPA, linking low-frequency activation to amyloid plaques and high-frequency activation to neurofibrillary tangles, shedding light on the underlying mechanisms of cell death in the brain.
 Prior to this study, it has been unclear whether reductions in brain activity seen in PPA are solely due to brain atrophy or if independent factors are at play. Hinkley notes that merely observing reduced brain activity doesn't provide a complete picture. "By looking at atrophy and brain activity, we can identify that there are reductions in brain activity independent of atrophy, meaning that if you have reduced neural activity in a certain part of the brain, which can be characteristic of the disease, it's not just due to the atrophy." This is important because PPA is often diagnosed only after significant atrophy has occurred. Identifying patterns of brain activity independent of atrophy could potentially enable the detection of the disease in its early stages, before behavioral symptoms manifest.
Prior to this study, it has been unclear whether reductions in brain activity seen in PPA are solely due to brain atrophy or if independent factors are at play. Hinkley notes that merely observing reduced brain activity doesn't provide a complete picture. "By looking at atrophy and brain activity, we can identify that there are reductions in brain activity independent of atrophy, meaning that if you have reduced neural activity in a certain part of the brain, which can be characteristic of the disease, it's not just due to the atrophy." This is important because PPA is often diagnosed only after significant atrophy has occurred. Identifying patterns of brain activity independent of atrophy could potentially enable the detection of the disease in its early stages, before behavioral symptoms manifest.
Implications for Patient Care
This study underscores the limitations of physicians and neurologists relying solely on traditional behavioral assessments to diagnose neurological diseases. Integrating advanced imaging provides a more comprehensive understanding of these conditions, aiding in better categorization and potentially opening the door to new therapies and clinical trials. For patients and their families, this study offers hope for more accurate diagnoses and a clearer picture of what to expect during disease progression.
Hinkley noted the significance of UCSF facilities for patient care: "There are only a few dozen MEG machines scattered across the US, and we are fortunate to have one of the few on the West Coast at UCSF. We use it a lot for surgical mapping, pre-surgical mapping and patients with a tumor or epilepsy because it has that precision."
Future Research Directions
"We want to move forward into designing additional investigations combining different imaging techniques," Hinkley noted, such as positron emission tomography, magnetic spectroscopy, and EEG to gain a more comprehensive understanding of neurodegenerative diseases. Hinkley added, "This study was one part of a larger series of studies that we have in collaboration with Marilu Gorno-Tempini at the Memory and Aging Center." The team is also exploring transcranial magnetic stimulation, a neuromodulation technique, to stimulate brain activity in areas affected by disease.
By combining advanced imaging techniques in novel ways and challenging the conventional view of neurodegenerative diseases, UCSF researchers like Hinkley and his collaborators are advancing our ability to diagnose and treat patients with these conditions more accurately.
