UCSF Breast Imaging Experts Advise Annual Screening Mammograms
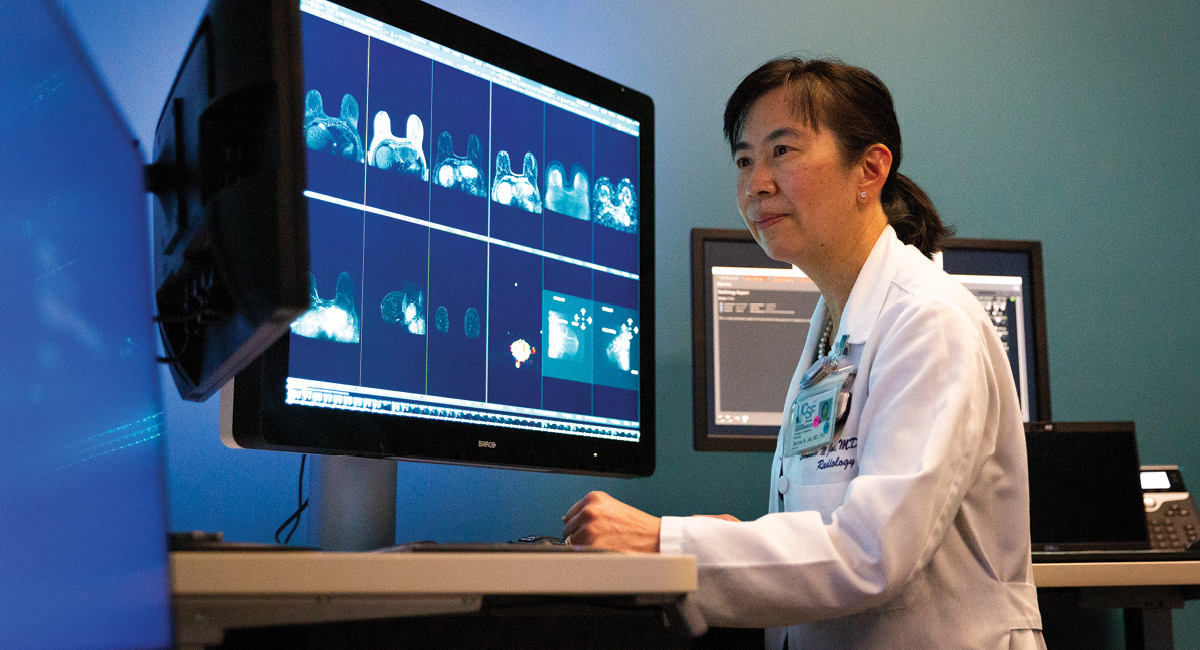
The U.S. Preventive Services Task Force (USPSTF) recommends that women begin breast cancer screening mammograms at age 40 and continue to have mammograms every two years (biennially) thereafter. Bonnie Joe, MD, PhD, Breast Imaging Division Chief at UCSF’s Department of Radiology and Biomedical Imaging, contends that biennial screening mammograms are not frequent enough and recommends that the standard should be annual screenings. Her recent editorial, “Annual Mammography Saves More Lives and Minimizes per-Mammogram False-Positive Results” published in the journal Radiology, expands on the comments Joe and Kimberly Ray, MD submitted when the USPSTF draft recommendations were made public in 2023.
There has been a longstanding debate over when to begin breast cancer screenings and how often to screen. In 2009, the USPSTF raised the suggested age of first screening from 40 to 50, and thereafter every two years. The recommended age was reverted to 40 in 2023, in agreement with the American College of Radiologists, but did not concur with the ACR’s recommendation to return the screening standard to annual mammograms. Joe believes that the downward revision on screening age minimums is a correct step, but the biennial recommendation fails women at risk for highly aggressive cancers.
As Joe said, “It is disappointing that the USPSTF did not come out in full support of annual screening, particularly if their goal is to reduce health care disparities. Annual screening from ages 40 to 79 years results in the highest mortality benefit and life-years gained and the lowest false-positive rate per screening examination of all the screening scenarios.”
Joe is by no means alone in her stance, as she referred readers to a study by Monticciolo et all, published in that same issue of Radiology, which compared the benefits and risks of screening scenarios starting at age 40 versus 50 years and using annual versus biennial screening intervals, using modeling from the Cancer Intervention and Surveillance Modeling Network, and data from the Breast Cancer Surveillance Consortium and from the Surveillance, Epidemiology, and End Results program. This study found that annual screening scenario would result in a 39% relative improvement in mortality reduction over biennial screening at ages 40–74 years, per current 2023 USPSTF recommendations.
The benefits are even more striking for Black women. Joe explained that the authors found that 65 life-years would be gained for annual screening at ages 40–79 years when compared with biennial screening at ages 40–74 years. For Black women, the estimates were 80 life-years gained with such annual screening gained for biennial screening. In her editorial, Dr. Joe called attention to studies which show Black women have a higher risk of dying of breast cancer and frequently have more aggressive cancer. Black women would benefit from increased frequency of testing, according to these facts noted in the USPSTF report but not actioned on in its final recommendation.
These different screening recommendations create friction between radiologists following “annual at 40” ACR recommendations and referring primary care providers following “biennial at 50” USPSTF recommendations.
Joe advocates for a more rigorous standard, “It seems safest to follow the 2021 updated ACR recommendations for every woman to undergo breast cancer risk assessment by age 30 years and, if of average risk, start annual screening at age 40 years and continue past 75 years unless severe comorbidities limit life expectancy.”
