UCSF Radiology's Role in the Multidisciplinary Approach to the Placenta Service (MAPS) at UCSF
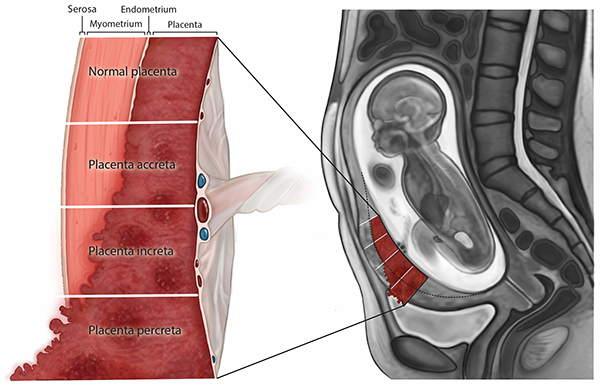
The UCSF Multidisciplinary Approach to the Placenta Service (MAPS) plays an important role in the diagnosis and management of pregnancies complicated by placenta accreta spectrum (PAS) disorders. Placenta accreta spectrum (PAS) disorders occur when the placenta attaches too strongly onto, or too deeply into, the uterine wall. Radiologists from the Abdominal Imaging/Ultrasound and Interventional Radiology sections, technologists, sonographers, and nurses in the UC San Francisco Department of Radiology and Biomedical Imaging are part of the large collaborative team.
Incidence of PAS disorders have increased dramatically – quadrupled since the 1980s – primarily due to the rise in rates of birth by cesarean section. Pregnancies complicated by PAS disorders can have potentially life-threatening consequences for both the mother and infant, particularly if the diagnosis of PAS has not been established prenatally. The diagnosis, management and postpartum care for PAS disorders require a multidisciplinary team approach that draws expertise from across the medical center focused on optimizing safe outcomes for mothers and babies.
UCSF’s Multidisciplinary Approach to the Placenta Service (MAPS)
The UCSF MAPS team uses a multidisciplinary approach to diagnose and care for pregnant women with PAS, who are at high risk for peripartum complications. Diagnosis of PAS, in most cases, is first suspected on an obstetric sonogram. Upon referral, evaluation at UCSF starts in the Radiology Department, where targeted scans are done to evaluate the placenta and uterus. The imaging studies (sonograms and, in most cases, MRI exams) are interpreted by UCSF Radiology faculty members with particular interest and expertise in this entity. Our growing experience with characteristic, atypical and sometimes subtle findings of this high-risk condition has enhanced our ability to confidently recognize PAS and offer information about degrees of invasion.
The findings are reviewed with colleagues who specialize in maternal-fetal medicine/high-risk obstetrics. The results and clinical plan are discussed with the patient and her family. When PAS is suspected or confirmed by imaging, patients are closely followed by our team which includes gynecologic/oncologic surgeons, anesthesiologists, neonatologists, nurse coordinators from the obstetric service, operating room and neonatal care unit. Multiple meetings, referred to as “huddles,” are held to coordinate pregnancy care and prepare for an optimized safe delivery.
Regular “huddles” to address patient needs and work toward continued improvement
Regular “huddles” are made up of specialized groups often with more than 20 participants from different departments, including Radiology, to discuss each case and to review findings and address the potential needs of the patient and her family. The obstetric sonograms and MRI scans are presented, after which a detailed checklist is used to identify key personnel, confirm anesthesia and surgical plans, and discuss staffing and operating room requirements. The checklist ensures a systematic approach to the care of each MAPS patient and permits identification of small adjustments that can result in significant improvements to the process.
Information from every MAPS delivery is carefully recorded, including surgical details, postoperative course and findings at pathology. The multi-disciplinary MAPS team holds routine de-briefing meetings. Feedback is essential to increasing the accuracy of our diagnoses and the success of our outcomes.
Establishing a pathway for safe delivery
The team of MAPS providers has grown to rely on the accurate interpretation of these challenging high-stakes studies by UCSF Radiology. In such cases the obstetric care plan involves cesarean-hysterectomy whereby the infant is delivered via C-section, the placenta remains attached, and the uterus is then surgically removed. Intra-operative US to “map” the placenta prior to uterine incision is now routinely performed in these cases. There is longstanding experience with this application of US as the UCSF Fetal Treatment Center is the birthplace of in utero surgery.
Our UCSF Radiology faculty determine where to enter the uterus to safely access and deliver the infant. Following ultrasound-guided hysterotomy (incision into the uterus), the baby is delivered and cared for by the Neonatology team. The placenta is left in place and the uterus is then closed by the OB/GYN surgeons in preparation for the next step. To minimize bleeding, the patient undergoes uterine artery embolization (UAE), performed by UCSF interventional radiologists.
The uterine arteries are selectively embolized to limit blood flow to the uterus and pelvis. To accommodate this complicated time urgent sequence of events, these cases are often done in a dedicated hybrid operating suite, equipped for both surgical and IR procedures. Immediately following UAE, the surgeons perform a hysterectomy, removing both the uterus and placenta in situ.
Research to identify, define and refine knowledge about PAS
UCSF radiologists have also conducted research that has been instrumental in identifying, defining and refining knowledge about PAS. Priyanka Jha, MBBS, associate professor of clinical radiology, and Liina Poder, MD, professor and director of ultrasound in the Abdominal Imaging Clinical Section were lead authors on important consensus work from the Society of Abdominal Radiology (SAR) and European Society of Urogenital Radiology (ESUR). They created joint guidelines and proposed strategies to standardize image acquisition, interpretation and reporting of imaging studies in patients with PAS. Dr. Poder was also part of an expert panel that recommended classification and reporting guidelines for the pathology diagnosis of PAS disorders.
Our team’s interest in imaging manifestations of PAS in conjunction with ongoing improvements in MRI technology have allowed for new insights into useful, clinically relevant findings. UCSF MAPS radiologists including Dr. Jha, Ruth Goldstein, MD, Stefanie Weinstein, MD, Tara Morgan, MD, Dorothy Shum, MD and Michael Ohliger, MD, PhD were part of a multidisciplinary UCSF team that reported on the “placental bulge sign” indicating myometrial invasion in PAS disorders. This sign is one of several imaging findings that carries high specificity for the diagnosis of this condition.
Accurate prenatal detection with high-quality imaging and expert interpretation, along with carefully coordinated efforts by multiple specialists to establish a delivery plan tailored to the circumstances of each patient form the foundation of our service, which is committed to the health and well-being of mothers and their children.
A full version of this story appears in Images Magazine, our department’s annual publication. Thank you to Drs. Jha, Poder, Vickie Feldstein, MD, renowned leader in ultrasound and professor of clinical radiology, and Mark Sugi, MD, assistant professor of clinical radiology. All are MAPS team members who were instrumental in putting this article together.
View current and past issues here.
