Which Imaging Exam is Ideal for the Diagnosis and Treatment of Epilepsy?
Epilepsy is a common and disabling disorder caused by the unpredictable and uncontrolled electrical discharges within the brain. Imaging is an essential tool for the evaluation and management of patients with this disabling condition. If you have epilepsy and have been referred for imaging, there are several radiologic tools that might be used in your treatment planning:
MEG (Magnetoencephalography)
MEG uses sensors to noninvasively detect and record minute magnetic fields associated with brain activity. The technique works like a very sensitive microphone that records magnetic fields emitted by brain cells instead of sound. Most patients can rest during an MEG, though in some cases the patient will perform simple tasks to stimulate certain areas of the brain. This exam provides timing – down to the sub-millisecond – as well as spatial information about brain activity.
EEG (Electroencephalogram)
An EEG is the most common test used to evaluate patients with epilepsy. In contrast to MEG, which detects magnetic fields related to neuron activity, EEG detects electric fields produced by neurons in your brain. Information from these two tests is complementary, and can be collected at the same time in order to gather reference information about where the brain activity is coming from.
MRI (Magnetic Resonance Imaging)
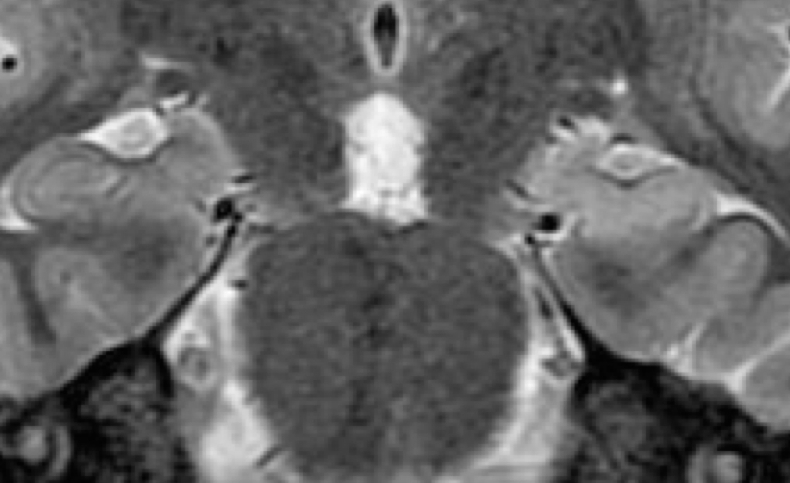
Epilepsy treatment is most effective when the onset of the seizure can be specifically localized to one or more origins within the brain. MRI collects structural information and creates images of the brain by using a large magnet. It is the most important imaging modality for epilepsy evaluation. Because of its critical role in management, MRI should be performed using a state-of-the-art 3 tesla MRI scanner according to technically specific scan protocols. The MRI should also interpreted by subspecialty-certified neuroradiologists with expertise in epilepsy.
MSI (Magnetic Source Imaging)
MSI combines MEG, EEG and MRI to create functional maps of brain activity that are more accurate than MEG or EEG alone. These maps can show where areas of normal and abnormal activity are located. The technique can also map areas of function (including language, hearing, touch, movement and more) in patients scheduled for surgery in order to help surgical planning and navigation.
PET (Positron Emission Tomography)
A PET scan may also be used to localize parts of the brain causing seizures. While an MRI uses a magnet, a PET scan involves injecting a small amount of low-dose radioactive substance, usually FDG. This results in images of the brain’s basic biochemistry or function that are sensitive to abnormal neurons. At UCSF, PET technology is combined with computed tomography (CT), thereby increasing diagnostic accuracy and specificity by allowing the information from two different studies to be correlated and interpreted on one image.
SPECT (Single-Photon Emission Computed Tomography)
SPECT is a nuclear medicine procedure which uses radioactive compound to create 3D images of cerebral blood flow. SPECT can be performed between seizures (interictal) or during a seizure (ictal) to assess blood flow patterns and thereby identify where the seizures are coming from.
Diagnostic and treatment planning for epilepsy will depend on a number of factors and may include multiple types of imaging exams. Your epilepsy team should consist of a neuroradiologist and epileptologist working with neurosurgeons, neuropsychologists and other epilepsy specialists from initial evaluation through and beyond surgery.
At UCSF, our Neuroradiology Research Group is conducting research to find new approaches for the diagnosis and evaluation of epilepsy and other neurological conditions. Learn more here or call to schedule an appointment to learn more about the radiological techniques that can be used to diagnose or treat epilepsy.
