CT-Guided Interventional Spine
Minimally invasive techniques are used to diagnose and treat vertebral disc problems and many other conditions of the spine. Imaging technology precisely guides minimally invasive procedures with needles, catheters and other devices. Our team of world-renowned neuroradiologists specializes in spinal and nerve diagnosis and interventions.
UCSF Precision Spine and Peripheral Nerve Center
Patients from throughout the San Francisco Bay Area are referred to the UCSF Precision Spine and Peripheral Nerve Center, which combines both the latest diagnostic spine magnetic resonance and low radiation dose 64 slice computed tomography services with innovative image-guided therapeutic pain management services. UCSF is the only university medical center in Northern California to offer CT-guided advanced spine treatment techniques.
Highlights
- The highest resolution scanners available, including two state of the art 64-slice computed tomography (CT) scanner that is dedicated full time to spine treatment and equipped with the latest radiation dose reduction software. The Adaptive Statistical Iterative Reconstruction (ASIR) software is the first software to dramatically reduce—from 50 to 80 percent—the patient’s radiation dose while also sweeping noise from and improving the quality of CT images.
- The highest quality and widest range of diagnostic and interventional spine services available in the San Francisco Bay Area.
- Internationally regarded neuroradiologists, who perform all procedures and interpret all diagnostic studies.
- Dedicated nursing and technologist staff who specialize in maximizing the efficacy and safety for all patients undergoing spine treatment services.
- Low-dose CT and X-ray fluoroscopy technique to minimize patient radiation exposure during spinal procedures.
- A convenient location, across from AT&T Baseball Park in San Francisco, that is easily accessible by car, UCSF shuttle, Caltrain, and Muni.
Conditions Diagnosed and Treated
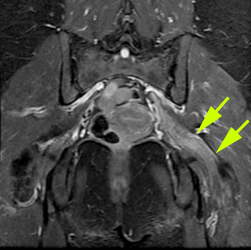
World-renowned neuroradiologists at the UCSF Precision Spine and Peripheral Nerve Center diagnose and treat the following causes of back, neck, arm, leg and hip pain, as well as peripheral nerve disorders:
- Degenerative Disc Disease
- Disc Herniations and Osteophytes
- Synovial Cysts
- Peripheral Neuritis
- Spinal Stenosis
- Spinal Deformity
- Vertebral Compression Fractures
- Sacral Insufficiency Fractures
- Spinal Tumors
- Piriformis Syndrome
- Cerebrospinal Fluid (CSF) Leaks
- Facet and Sacroiliac Joint Disease
- Tarlov Cysts
Innovative Spine Procedures
CT- guided procedures may be particularly helpful for patients who:
- Have had extensive surgery with hardware that obscures or distorts the usual spinal anatomy.
- Have significant osteoarthritis that may hinder access to nerves and other spinal structures.
- Have soft tissue abnormalities such as disc herniations, cysts or scarring from prior surgery that are not visualized using conventional fluoroscopy-guided techniques.