Thyroid Radiofrequency Ablation (RFA): A Minimally Invasive Alternative to Thyroidectomy
Benign thyroid nodules are a common condition present in up to 80 percent of the population. The vast majority (greater than 90 percent) of nodules are typically benign. Although benign, they often can be felt and seen when they become large. Additionally, they may lead to symptoms such as difficulty swallowing, hoarseness, and general neck discomfort as they grow.
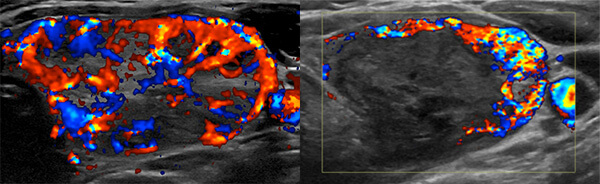
Radiofrequency ablation (RFA) is a minimally invasive method of shrinking tumors using heat energy to destroy tissue. It has been applied by Interventional Radiologists under real-time image-guidance for many decades to treat cancers in the lung, liver, and kidney as an alternative to invasive surgical resections. RFA of the thyroid has been shown to be a safe and effective alternative to surgery to decrease size and improve symptoms associated with benign thyroid nodules.
Thyroid RFA is offered to our patients as a collaborative effort between UCSF Interventional Radiologists, Ultrasound Radiologists, Endocrinologists, and Endocrine Surgeons. Our multidisciplinary approach allows us to individualize care to patients and ensure optimal, comprehensive management before, during, and after your procedure.
Why choose RFA?
Compared to surgery, RFA has been shown to spare more normal thyroid tissue leading to a decreased risk of developing post-treatment hypothyroidism (low thyroid hormone), which may require long-term hormone supplementation. RFA has also been associated with improved patient satisfaction, better quality of life, and lower risk of adverse events with similar improvement in symptoms. Scars are also not present after RFA and recovery tends to be faster.
In patients with hyperfunctioning thyroid nodules (also known as autonomously functioning thyroid nodules, or AFTN), RFA can also be considered as an alternative to radioactive iodine (RAI) treatment, which is typically given as an oral medication and requires isolation for approximately 1-2 weeks while the patient remain radioactive. If a patient is unable to isolate from others (for example, to care for a child or go to work), RFA is an alternative to consider.
Who is a good candidate for this procedure?
RFA is suitable for patients with cosmetic concerns and/or symptoms associated with their benign thyroid nodules. Thyroid nodules that are solid (or predominantly solid) and proven to be benign following biopsy are appropriate for RFA. Hyperfunctioning thyroid nodules can also be appropriate for RFA.
Patients with cystic (or predominantly cystic) nodules are often better treated with ethanol ablation. In the event of recurrence after ethanol ablation, treatment with RFA could be considered.
There is not an absolute size threshold where thyroid RFA is not offered. However, larger nodules may require more than one ablation to achieve an appropriate size reduction.
Pregnant patients, those with cardiac pacemakers, and those with biopsy results other than benign are not appropriate candidates for RFA.
What are a patient’s expectations surrounding the procedure?
Thyroid RFA is an outpatient procedure that typically takes approximately 60-90 minutes depending on the size of the nodule being treated. Patients are given the option of sedation through an IV for comfort versus local anesthesia. Nonetheless, patients are typically awake the entire time during the procedure.
After the procedure, a small bandage is placed over the access site. Patients typically leave after 1-2 hours of recovery. Mild bruising and soreness are expected the first few days after the procedure which can be managed with anti-inflammatory medications and an icepack.
Overall risks are low, but include bleeding, infection, and damage to the nearby nerves. These will be further discussed in consultation.
Patients typically report a size decrease and improvement in symptoms within 1 month. The decrease in size often continues for about 6 months after the procedure. Ultrasound scans are performed after the procedure in regular intervals followed by a clinic follow-up. If symptoms remain or the nodule does not shrink appropriately, as can occur with larger nodules, repeat ablation can be considered.
Will insurance companies cover thyroid RFA?
Thyroid RFA is a novel procedure for managing patients with benign thyroid nodules. As such, coverage by insurance companies, although not universal, continues to increase as more studies are published demonstrating its safety and effectiveness. Our staff will work with your insurance provider to understand if the procedure is covered. If not, alternatives are available to ensure that you are able to get the care you need.
How can I be evaluated for thyroid RFA?
If you are interested in learning more about thyroid RFA, please contact our staff to set up an appointment for consultation. Alternatively, you may reach out to your care team to place a referral to UCSF Interventional Radiology. From there, our staff will work with you directly to schedule the consultation.
- UCSF Interventional Radiology
Phone: (415) 353-1300
Fax: (415) 353-8570 - How to refer to UCSF Interventional Radiology


