BI-RADS and Breast MR: How Well Are We Managing Patients Based on Established Standards?
Our latest research, published in the January 2016 edition of American Journal of Roentgenology, suggests that there is room for improvement by radiologists when it comes to managing patients in accordance to established BI-RADS categories for breast MRI exams.
 What is BI-RADS?
What is BI-RADS?
The American College of Radiology established a standardized reporting system, called the Breast Imaging Reporting and Data System (BI-RADS), to describe breast imaging findings and results on mammography, ultrasound, and MRI. The concept of BI-RADS was first developed for mammography in the early 1990s to address the problems of variable and ambiguous reporting practices as utilization of this modality increased. Since its inception and evolution, BI-RADS has become central to the practice of breast imaging. An important component of this reporting system is a defined assessment category, numbered 0 through 6 based on the likelihood of malignancy, and a corresponding clinical management recommendation to be used with each assessment category. Use of this common language in breast imaging reports allows radiologists to clearly communicate diagnostic conclusions and recommendations to the patients’ primary physicians, surgeons and oncologists across practices.
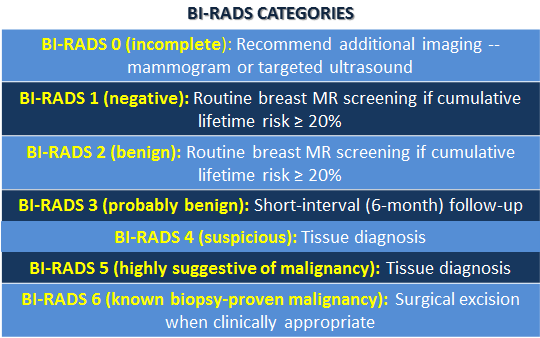
- BI-RADS 0 (incomplete): Recommend additional imaging — mammogram or targeted ultrasound
- BI-RADS 1 (negative): Routine breast MR screening if cumulative lifetime risk ≥ 20%
- BI-RADS 2 (benign): Routine breast MR screening if cumulative lifetime risk ≥ 20%
- BI-RADS 3 (probably benign): Short-interval (6-month) follow-up
- BI-RADS 4 (suspicious): Tissue diagnosis
- BI-RADS 5 (highly suggestive of malignancy): Tissue diagnosis
- BI-RADS 6 (known biopsy-proven malignancy): Surgical excision when clinically appropriate
MRI & BI-RADS
While BI-RADS was initially used for communication in mammography, in 2003 the system was adapted to use with breast MRI, as the use of MRI for breast cancer detection and characterization has increased dramatically over the past decade. The breast MR categories were most recently updated in 2013.
Prior to our research, very little was known about how BI-RADS assessment categories and associated management recommendations have actually been used in routine clinical practice in the United States. This is important to know, since BI-RADS assessment categories and recommendations have become the standard by which we communicate breast imaging results to referring physicians so that they can determine the appropriate care for their patients.
Research Findings
My colleagues and I assessed how often patient management recommendations were concordant with the reported BI-RADS categories pictured below. We analyzed data from 8,283 breast MR exams from four regional registries in the Breast Cancer Surveillance Consortium (BCSC) for the years 2005 to 2011. The BCSC comprises a large sample of patients, radiologist, and imaging facilities across diverse geographic and practice settings, and has been shown to be a broadly representative cross section of the national population. We found that overall concordance between BI-RADS assessment categories and radiologists’ management recommendations was moderate at 77 percent. The highest agreement was in exams with BI-RADS categories of 1 and 2, while exams categorized as BI-RADS 3 or 6 had the lowest agreement at 36% and 56%, respectively.
The high concordance in the reporting of recommendations for BI-RADS assessment categories of 0, 2, 4, and 5 shows that radiologists are using the BI-RADS categories as intended in these cases. But the low concordance for BI-RADS assessment categories 3 and 6 demonstrates a need for further improvement- and focused education in those areas.
It’s clear that BI-RADS 3 for breast MR has been a source of confusion, perhaps because data assigned to the category is limited. With BI-RADS 6, we believe the low concordance is due to the lack of understanding about the appropriate use of the category. Moving forward, it’s necessary to further educate radiologists about the appropriate scenario in which each category and recommendation should be used. With further education, we hope to see improved reporting of concordant BI-RADS assessments and management recommendations to better facilitate the care of patients undergoing breast MRI.
To learn more about this research, read more from AuntMinnie.com. Click here for more information about BI-RADS and regular breast screening.

