MR Enterography in Children: A Non-Radiation Exam of the "Smaller" Bowel
The following article was written by Jesse Courtier, MD, Assistant Clinical Professor of Pediatric Radiology at UCSF.
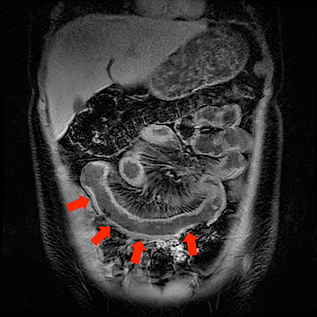
Inflammatory bowel disease (IBD) (including Crohn’s disease and Ulcerative Colitis) affects both adults and pediatric patients with an estimated 10,000-47,000 new cases diagnosed each year. Up to 1/3rd of these cases are in the pediatric population [1,2]. This condition causes inflammation of the small and large bowel, leading to complications such as infection and bowel obstruction. Patients will endure bouts of remission interrupted by acute flares of inflammation. This can lead to multiple visits to the emergency department. More often than not, imaging is also performed during these visits. In a patient with IBD, these patients may undergo multiple imaging examinations over the course of their lifetime. In a pediatric patient with this diagnosis, the number is even greater. It is for this reason that any exposure to ionizing radiation should be minimized and alternative non-radiation methods should be employed whenever possible. MR enterography, a non-radiation method of examining the bowel, has recently emerged as highly effective method of assessing disease in these patients.
MR enterography uses Magnetic Resonance Imaging (MRI) with oral and intravenous contrast to assess the entire abdomen and pelvis including the bowel. This allows the radiologist to see processes both inside and outside the bowel, all without the use of ionizing radiation. At the UCSF Benioff Children’s Hospital, we have optimized our MR enterography examination to evaluate patients across a broad age range. This even includes the addition of flavor additives to our oral contrast to improve taste of the oral contrast!
Recently we have implemented a "Child Life" MR enterography protocol for our youngest patients. This is a tailored protocol performed with the aid of our Child Life Specialists on a magnet equipped with MRI video goggles. Using this team-effort, we are able to perform this examination without the use of anesthesia on children as young as 5 years of age. This is a specialized approach that is unique to our center.
Our section also works very closely with the Pediatric Gastrointestinal division here at the UCSF Benioff Children's Hospital discussing complex cases on a routine basis. Using our team-orient approach we continually strive to provide the best in imaging for our pediatric patients with known or suspected inflammatory bowel disease!
Questions or comments? Post them in the discussion section!
REFERENCES:
1. Loftus EV. Clinical epidemiology of inflammatory bowel disease: Incidence, prevalence, and environmental influences. Gastroenterology 2004 126:1504-1517
2. Diefenbach KA Breuer CK. Pediatric inflammatory bowel disease. World J Gastroenterol 2006. 12: 3204-3212