Ultrasound-Guided Injection Relieves Pain, Enables Mom to Care for Newborn
Maryana was over-the-moon to be a mom for the first time when she learned she was pregnant in May 2022. Energetic and lively, Maryana was taken by surprise when she began experiencing difficulties halfway into her pregnancy.
At 16 weeks, the 32-year-old tech sales executive from Marin was diagnosed with severe symphysis pubis dysfunction (SPD), which refers to pain caused by pubic symphysis separation – the loosening of the joint between the left and right pelvic bones that occurs during pregnancy to allow the pelvic bones to widen during birth. Due to the pressure of her growing baby weighing on her pelvis, Maryana was in pain, the kind of pain that prevented her from walking up and down stairs. At 30 weeks, she was basically confined to her bed.
Maryana counted down the days until her due date. She believed everything would be better, once her baby was safely delivered. Doctors had advised – and her own Google searches confirmed – that in most cases this condition would go away shortly after birth. Determined to get through her pregnancy, Maryana pushed aside her feelings of fear and isolation.
She had no idea her toughest health battle would only just begin after she gave birth to Emily, a healthy baby girl, on December 27, 2022.
Maryana returned home from the hospital with her newborn, strong pain medication, and unbeknownst to her, pelvic pain (caused by pubic symphysis separation) that would be so debilitating once the medication wore off that she’d be confined to a wheelchair for nearly a month.
The Worst Day
“It was the worst and most shocking day of my life,” Maryana said about the day she stopped taking opioid pain medication and began breast feeding. The mind-blowing pain meant she could not walk, or even stand. “My legs were literally not holding me. My daughter is five feet away from me, crying in her crib, and I can’t get up. It is forever ingrained in my body how horrible that was.”
Maryana knew something was very wrong. She received an X-ray at the hospital, but it did not show the structural bone damage that had occurred to her pelvis because she was lying down for the procedure. Later, Maryana learned she suffered from traumatic separation of the pubic symphysis, the joint that holds the pelvic bones together, and bone marrow edema, a bruising of the pelvic bones.
Maryana’s condition was far worse than anyone expected, and to her shock, it seemed no one knew what to do. She felt like a hot potato being passed from clinicians in obstetrics, to pain management, to orthopedics. Unfamiliar with the severity of her injury, doctors waited weeks for insurance authorizations for each step of the evaluation process, as well as scheduling delays. Maryana was left with a deep sense of distrust. How could she have access to what felt like all the resources in the world, and yet no one was able to help alleviate her condition so she could fully care for her newborn baby? She was taking Advil and Tylenol daily to manage the pain, but she was still only able to walk from her bed to her bathroom most days.
Searching for answers, Maryana was referred to University of California, San Francisco (UCSF).
UCSF’s Breadth and Depth of Specialty Care
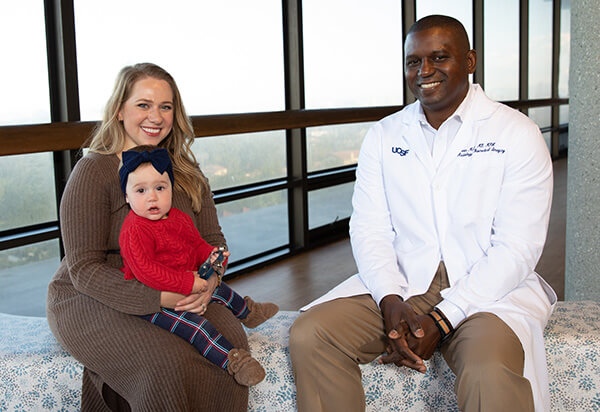
Here, with the breadth and depth of expert care, two specialists teamed up to get Maryana the help she needed. Melanie M. Henry, MD, MPH, FASA, an anesthesiologist, pain management specialist, professor, and Director of Telehealth and Outreach at UCSF Health, collaborated with Kevin McGill, MD, MPH, an assistant professor of musculoskeletal imaging and the Director of Musculoskeletal Interventions in the Department of Radiology and Biomedical Imaging. “I was hardly able to get to the chair for my video call,” said Maryana, who met Henry for a telehealth visit about one month after she gave birth. Once they talked, she felt seen for the first time. With emotion choking her words, Maryana described the feeling of “being taken into warm arms” as she heard Henry’s first words: “I am a mother too, and I am so sorry you are going through this.”
“For Dr. Henry to see me as a human and a mother – it brings tears to my eyes to know what she did for me in that moment.” After connecting with Henry, everything started to change. After a series of evaluations, Henry contacted her colleague McGill, who specializes in image-guided joint interventions.
“Dr. McGill is an angel. He put me back on my feet, quite literally,” said Maryana, who to this day shares photos of Emily with him. “He forever has a piece of my story and my heart.”

The Role of the Radiologist
“When I initially met Maryana, she was in a lot of pain and desperate for a solution. I recommended she come in for a diagnostic ultrasound with our expert musculoskeletal sonographers. After the images were obtained and a subsequent neurogram was performed, I had a conversation with her about her condition and the procedure,” said McGill, who performed an ultrasound guided steroid injection into Maryana’s pubic symphysis to relieve her pain. Though she had an initial bad reaction called a steroid flare, it did not impact her recovery.
“She handled the procedure remarkably well. I called her the next day to see how she was doing. The pain had not completely resolved at that time, but she seemed optimistic,” said McGill, who continued correspondence with Maryana over email and as her symptoms improved.
For the first time during her ordeal, Maryana felt like doctors genuinely cared about her care and how she was doing. “When the level of pain you are in is seen and believed, and a doctor reaches out to you unprompted, it changes everything about that experience,” she said.

Previously, Maryana imagined a radiologist as someone who sat in a dark room and looked at X-rays all day. Today, she continues to be amazed by the personal care and attention she received from McGill and the fact that a radiologist was the answer to her grave condition. “Dr. McGill has made a huge impact on my life. I am so grateful.”
“I am honored to have been given an opportunity to provide care for Maryana. She is the type of patient that reminds me why I chose a career in medicine,” said McGill, reflecting on this experience.
After receiving the injection, Maryana slowly got better, feeling more and more relief from the pain as the weeks progressed. After being nearly immobile for 6 months, she was able to move around more and more and continue with physical therapy to rebuild her muscles.
In early fall, about 10 months after giving birth, Maryana felt no more pain. She was able to take her daughter to the grocery store by herself for the first time. Although she realized her status is what most other moms experience at two weeks postpartum, she was elated to be able to fully participate in her daughter’s life, without mobility being an issue.
“Maryana was an advocate for herself and pursed all options to find the appropriate treatment. We all worked together, and Maryana allowed both of us to be the best physicians possible,” said Henry.
A Future Not Yet Written
“I don’t take for granted that I was able to go on a 15-minute walk yesterday,” said Maryana with renewed self-assurance and a sense of inner strength. She’s looks forward to chasing after her 1-year-old soon enough.

Her advice to others who may be experiencing a similar challenging condition is to keep searching until you find the right experts.
Once a self-described non-support group person, Maryana now turns to her community on Facebook of other people around the world who also experienced severe pubic symphysis separation. “Some have gone on to have other children and are ok, some need mobility aids permanently, and some have their pelvis bolted together afterwards,” said Maryana. “I have the providers, I know what to expect, but no one can tell me it will be ok.”
“Despite all this, becoming a mom is the best thing that ever happened to me. I’d go through it a million times over to have my daughter,” said Maryana. “She is my entire universe. The joy I get from seeing her grow is incredible.”
Symphysis Pubis Dysfunction (SPD)
 Symphysis pubis dysfunction (SPD) is a common condition that can lead to debilitating pain during pregnancy and in the post-partum period. The goals of treatment focus on decreasing pain while improving muscle function and joint stability using a combination of physical therapy, activity modification, a pelvic support belt, and/or oral medications. Alleviating pain in a timely manner is important to enable patients to adequately care for their newborns and/or return to work.
Symphysis pubis dysfunction (SPD) is a common condition that can lead to debilitating pain during pregnancy and in the post-partum period. The goals of treatment focus on decreasing pain while improving muscle function and joint stability using a combination of physical therapy, activity modification, a pelvic support belt, and/or oral medications. Alleviating pain in a timely manner is important to enable patients to adequately care for their newborns and/or return to work.
Diagnostic ultrasound is an excellent tool to assess pubic symphysis separation, which is often associated with SPD, in the peripartum period. If conservative measures fail, ultrasound is also the ideal modality for an image guided injection of anesthetic +/- steroids into the pubic symphysis for pain relief.
The rapid growth of the musculoskeletal ultrasound program at UCSF over the past few years has created wonderful opportunities for meaningful interactions with both patients and referring providers.
